Source(google.com.pk)
Blood And Cancer

In the battle against cancer, Dr. Judah Folkman (born 1933) has found a new approach: to attack the blood vessels that nourish cancer cells. The results of initial tests in cancer-bearing mice performed in 1998 were promising enough to raise the hopes of both cancer patients and physicians worldwide.
A noted professor, physician, and former surgeon-in-chief at the Boston Pediatric Hospital, Dr. Judah M. Folkman has demonstrated that by cutting off the blood supply nourishing cancer cells, cancer tumors can be killed with only negligible side effects. Theorizing on a method to prevent the growth of existing tumors, Folkman decided to try blocking the signals sent out by these tumors to perform angiogenesis - the formation of new blood vessels. To test his theory, he used two agents - angiostatin and endostatin - to treat cancer in laboratory mice. Although the results were positive, they were not conclusive, for other cancer-fighting drugs had a history of working well on mice but not as well on humans. By 2000 there remained the task of completing extensive tests on humans before Entre Med Inc., a Rockville, Maryland-based biotech company, could begin to put the new compounds on the market.
Discovered How Cancer Cells Grow
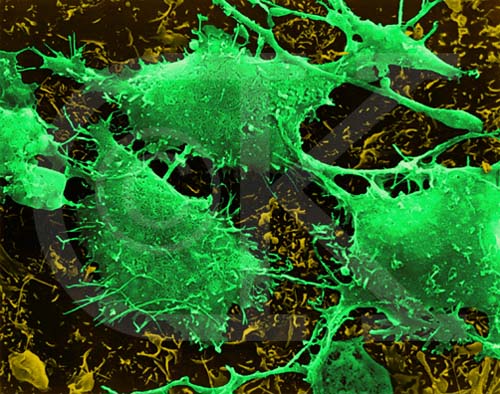
The son of Rabbi Jerome Folkman and his wife, Bessie, Folkman came to a love of medicine early in life. At his bar mitzvah his father told him to be a credit to his people; as an adult Folkman determined to dedicate himself to cancer research as a way of following his father's advice. In 1961 he made an astounding discovery. While doing medical research in a U.S. Navy laboratory, he found that cancer cells grow because they have an abundant blood supply. From this discovery Folkman developed the theory of angio-genesis and hypothesized further that cancers could not thrive without this abundant blood supply. A tumor formed, he theorized, because it could somehow stimulate new blood cells to deliver to it the nutrients it required in order to grow. Without sufficient blood, a cancer would not be able to grow any larger than a pin head.
Folkman's theory led him to look for ways to block blood vessel growth. He worked for years before he was able to develop compounds that sufficiently inhibited angiogenesis. These compounds, the human proteins endostatin and angiostatin, seemed like the answer to a prayer for people affected by cancer. Endostatin in particular showed promise; its marked lack of toxicity seemed to make it safe for human testing and two small-scale clinical trials at the U.S. National Cancer Institute (NCI) were authorized to further examine its effects on humans.
In February 1999, the NCI verified that Folkman's results with endostatin could be replicated. The human protein endostatin not only inhibited tumor growth in mice, but also showed no side effects when tested on in monkeys, even when administered in high doses. In an exciting announcement, the NCI confirmed that endostatin's anti-angiogenesis properties dramatically shrank cancerous tumors in laboratory mice.
The NCI's announcement came at the end of 30 years of arduous work on the part of Folkman. Years of work resulted in his discovery that blood vessels provided the key to cancer's survival, and much more research was subsequently undertaken in order for him to determine the basic process by which cancerous tumors spark the formation of the new blood vessels required to feed their growth. "Most research is failure," Folkman told NOVA producer Nancy Linde. "You go years and years and years, and then every once in a while there is a tremendous finding, and you realize for the first time in your life that you know something that hour or that day that nobody else in history has ever known, and you can understand something of how nature works."
Perhaps most frustrating for Folkman during his decades of research was the time it took him to convince the medical community that his theory had merit. Although he encountered skepticism from researchers, Folkman persisted because he knew that as a surgeon he had the hands-on experience with live human cancer tissues that researchers lacked. During surgery, Folkman had seen small tumors in the thyroid gland and the lining of the abdomen that never grew very large because they could not stimulate blood vessel growth. That led him to think that some kind of angiogenesis factor, possibly a diffusible protein, could stimulate the growth of blood vessels in certain tissues. But where the factor could not stimulate the formation of new blood vessels, the cancer did not grow. That meant cancer could be kept from growing if it could not attract the formation of a nutrient source. Folkman focused on determining what the factor was and if it could be blocked.
Discovered the Angiogenic Factor
Folkman maintains that being a researcher is one of the hardest jobs around, because, unlike a surgeon, a researcher doesn't get feedback from patients. That means that years of criticism, along with funding problems, must be faced before any positive reinforcement results from one's work. His own research experience was no exception to that rule. Fortunately, he was persistent; his knowledge as a practicing surgeon gave him the courage to continue presenting his ideas.
Although Folkman's ideas were at first largely discounted, by the 1970s that began to change. Researchers agreed that tumors did seem to cause the presence of new blood vessels, but most thought it was a side effect of dying cancer cells. They did not believe that the live cells actually stimulated the formation of new blood vessels.
When Robert Auerbach came to Folkman's lab, the two researchers conducted an experiment that proved the cancer cells were in fact causing the formation of blood vessels as a means of feeding their growth. Auerbach put live tumor cells in one eye of a rabbit and dying tumor cells in the other eye. The results showed that blood vessels formed around the live cells, not the dying ones. This proved that live cancer cells were actually causing the growth of the blood vessels.
In 1971 the New England Journal of Medicine published Folkman's paper that discussed the angiogenesis factor. Folkman began by noting that new blood vessels were recruited by tumors. Second, he maintained, the tumors sent out a factor that caused angiogenesis, or the formation of new blood vessels. Third, he said, this factor would stimulate the growth of new blood vessels. If this factor could be blocked, he hypothesized, tumors would stay small.
In 1984 Folkman and his team of researchers published a paper about the first angiogenic factor, a molecule that stimulated angiogenesis. He was later to discover 17 molecules, but the discovery of the first convinced him that he was on the right track. When he was unable to find the biological factor that stimulated blood vessel growth, Folkman began to wonder if he was being headstrong about his ideas rather than persistent. Realizing that he was right took time, but it was worth it in the end, when the medical community realized that through his work there was new hope for cancer patients: their disease could be stopped without debilitating side effects.
Experimented with Inhibitors
Killing cancer is a daunting task that often requires extensive drug treatments, chemotherapy, and radiation, which takes a heavy toll on healthy cells in the body. Cancer cells are more resistant to drugs than are normal cells, which is part of the reason why they are so hard to kill. The genius of Folkman's solution is that blood vessels are normal cells that respond readily to drugs. When subjected to angiostatin and endostatin treatments, blood vessels disappear, and with them, the tumors that feed on them. The anti-angiogenesis process might be compared to starving an enemy out by laying siege to his castle. No food supplies can get in, so the enemy eventually weakens. "We have been leveling out in our ability to stop cancer using available tools," Robert Siegel, director of hematology and oncology at George Washington University Medical Center, told Insight on the News: "The idea of having a completely new approach that is effective with some cancers is exciting."
Following testing on endostatin and its approval for use on human subjects, Duane Gay was one of the first to be treated with the substance. Although a tumor in his rib grew, those in his liver, lungs, and kidney stabilized. With the anti-angiogenic benefits of the drug interferon-alpha, Folkman also had successes treating children with hemangiomas, or life-threatening masses of blood capillaries. By the year 2000, 30 drugs were considered angiogenic inhibitors.
The Value of Observation
That Folkman perceived something no one else had noticed while working with cancer patients was not surprising to the people who know him best. Dr. C. Everett Koop, one of Folkman's colleagues at Boston Children's Hospital, found his colleague's power of observation startling. For example, when Folkman started in pediatric surgery, he had no experience working on young children. Koop painstakingly showed him the difference between pediatric tissues and adult tissues. While watching Koop, Folkman discovered that Koop's technique largely depended on steadying things with his left thumbnail against his left forefinger. Fingernails, Folkman decided, made all the difference. Koop had never realized how important his fingernails were before, but he knew Folkman was right.
Folkman's skill as a pediatric surgeon grew, as did his skill as a physician and researcher. He also becames a noteworthy professor whose students at Harvard Medical School counted him among their best teachers. Throughout the years Folkman conveyed to his students the importance of staying connected to patients. As a doctor, he gave his home telephone number and beeper number so that his patients could contact him. As a surgeon, he believed there was no such thing as "false hope." He advised his students never to tell a patient that there was nothing they could do to help him or her, because there was always something, even if it was only making the patient feel better.
In all his years of research, Folkman never lost sight of the people he was helping. Despite repeated criticism, he persevered with his assertions regarding cancer treatments until the medical community finally acknowledged that his research had in fact expanded their understanding of the disease. In fact, Folkman's research has applications for 26 diseases, including arthritis, cancer, Crohn's disease, endometriosis, and leukemia.
Robert Cooke, author of Dr. Folkman's War: Angiogenesis and the Struggle to Defeat Cancer, wrote that by 2000 Folkman's work was clearly recognized as having contributed to the sum of medical knowledge. "Finally it seemed that his peers were judging him to be persistent, not obstinate," Cooke wrote. "This was a distinction he had long sought. Now it seemed clear that great strides had been made largely because one man worked, pushed, and badgered one idea for so many years. Step by painful step, at first alone and then with colleagues he had engaged the struggle, Folkman had faced the objections and surmounted all the barriers that inflexible critics and doubters threw in his path. This experience had bred an enduring confidence and had even given him a sense of peace."
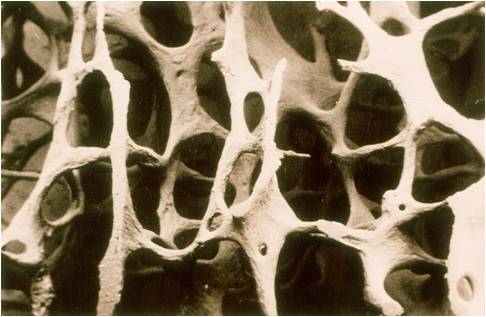
 Leukemia is a type of cancer which affects the bone marrow and is characterized by unrestrained proliferation of white blood cells. Its name “leukemia” means “white blood” since this cancer is characterized by a high number of white cells in the blood, many of which are immature or dysfunctional.
Leukemia is a type of cancer which affects the bone marrow and is characterized by unrestrained proliferation of white blood cells. Its name “leukemia” means “white blood” since this cancer is characterized by a high number of white cells in the blood, many of which are immature or dysfunctional.
 Leukemia is a type of cancer which affects the bone marrow and is characterized by unrestrained proliferation of white blood cells. Its name “leukemia” means “white blood” since this cancer is characterized by a high number of white cells in the blood, many of which are immature or dysfunctional.
Leukemia is a type of cancer which affects the bone marrow and is characterized by unrestrained proliferation of white blood cells. Its name “leukemia” means “white blood” since this cancer is characterized by a high number of white cells in the blood, many of which are immature or dysfunctional. In the battle against cancer, Dr. Judah Folkman (born 1933) has found a new approach: to attack the blood vessels that nourish cancer cells. The results of initial tests in cancer-bearing mice performed in 1998 were promising enough to raise the hopes of both cancer patients and physicians worldwide.
In the battle against cancer, Dr. Judah Folkman (born 1933) has found a new approach: to attack the blood vessels that nourish cancer cells. The results of initial tests in cancer-bearing mice performed in 1998 were promising enough to raise the hopes of both cancer patients and physicians worldwide..jpg) I started a new treatment in March, a week late, as I had to help move my grandma, since only one of her 6 children (plus 5 spouses) would help. My bf was going to help, but she changed the moving date, and he had already booked a day off for moving her.
I started a new treatment in March, a week late, as I had to help move my grandma, since only one of her 6 children (plus 5 spouses) would help. My bf was going to help, but she changed the moving date, and he had already booked a day off for moving her.























.jpg)








